Revenue Cycle Management
Revenue Cycle Management

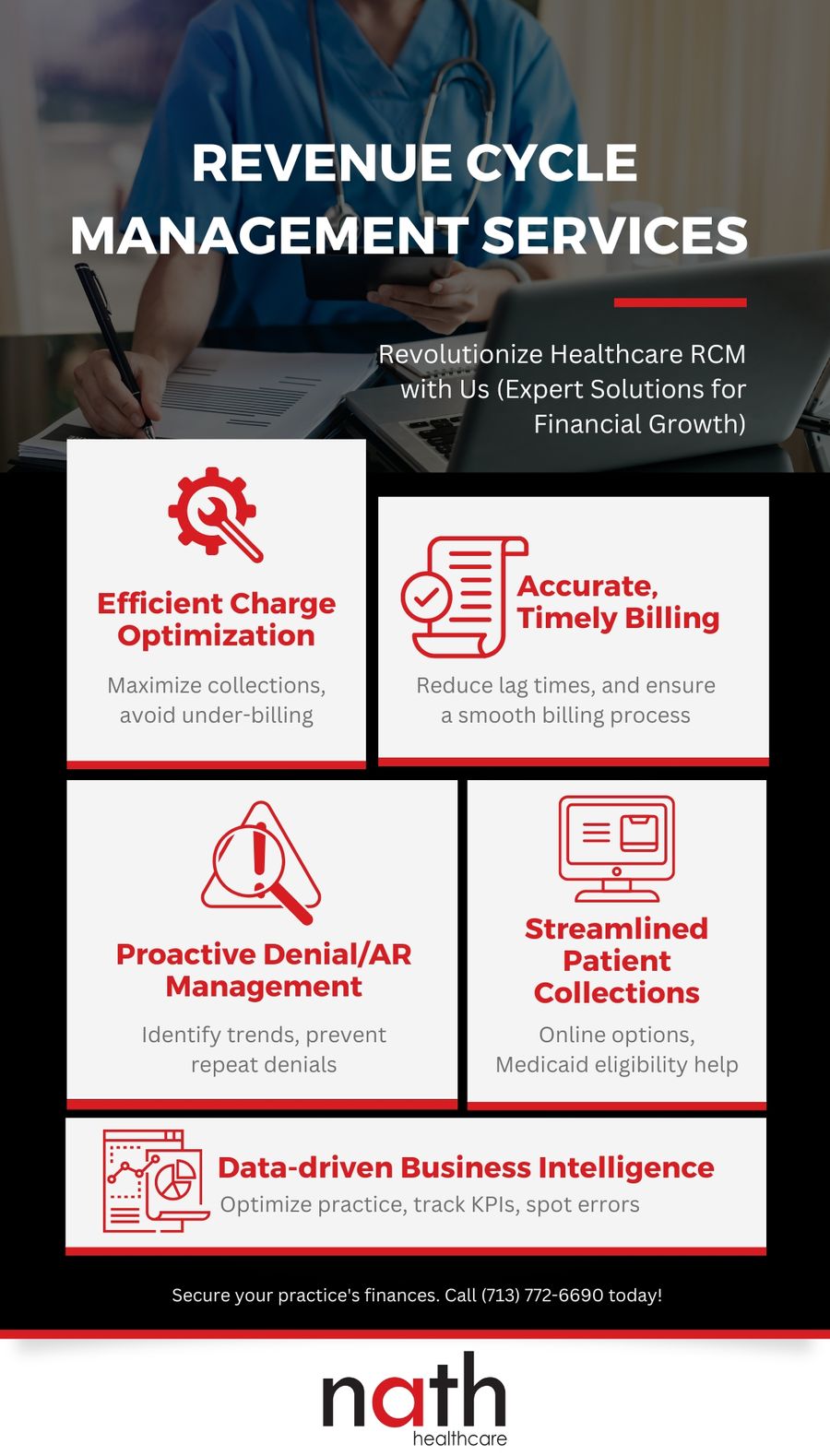
Our Revenue Cycle Management Services
At Nath Healthcare, we offer full-service revenue cycle services that maximize your collections. Our services ensure that your practice is armed with the best workflows, processes, and technology and are designed to capture revenue leakage at all areas of your practice including credentialing, insurance verification, coding, billing and patient collections. We get clients paid on the initial claims submission and implement continuous process improvements for denials.

What Sets Our Company Apart
As a healthcare service provider, our team recognizes that the demands of modern medicine must be met with a capable and efficient business organization. Medical professionals are increasingly burdened with managed care contracts, employee turnover, and administrative challenges, all of which can impact their abilities to treat their patients.
Our personalized and consultative approach to each client ensures that their revenue cycle management is optimized for efficiency and security. We prioritize people, processes, and technology to find the best solutions for each client's needs.
Contact us today to learn more about how our staff augmentation services can make a difference in your company!
